A 50 year old male who's a resident of nakrekal,labourer by occupation came to the opd to get admitted under de-addiction
CHEIF COMPLAINTS :
There were no specific complaints by patient but came for de-addiction
HOPI :
Patient was appareantly asymptomatie 4 years back ,then he developed
• Burning type of pain in the right and left hypochondrium,3 to 4 episodes for which he went to a local hospital and got medications(He's a chronic alcoholic), and the symptoms subsided,his last episode was the day after he got admitted here and was given pantop iv and the symptoms subsided.
• H/o weight loss approximately 20 kgs since 15 months
• 1 year back he was found to have high Sugars at a government camp at his place used OHA's for 4 months
• Then he developed complaints of Generalized weakness, polydypsia, poly urea for which he visited a private hosp at Nakrekal found to high sugars (Uncontrolled DM 2 ) He was on insulin(25 U) since then (took Insulin Irregularly) .
• Complaints of Diminution of vision since 8 months and double vision in the mornings since 7 months
• H/o light trauma 1 month back then he developed bubble like lesions associated with pain and itching for which he went to a local hospital and got some medications and pain and itching decreased but he was experiencing itching again since 29/7/22
• H/o Trauma (with mild skin abrations) 15 days back,then he developed itching over the wounds
Came to the opd and got admitted for de-addiction and was sent to GM for uncontrolled DM 2(550mg/dl)
• Complains of body pains since 3 days for which he was given tramadol
• Vomitings on 1/8/22 morning
2 episodes ,projectile type with food particles as content( early in the morning& after consuming milk) for which he's given medication and the symptoms subsided
• Burning type of pain the right and left hypochondrium and epigastric regions since 2/8/22
• Fever since 3/8/22
PAST HISTORY :
K/c/o DM 2 since 1 year
Not a K/c/o Hypertension ,asthma ,CAD, epilepsy, hypothyroidism
PRESENT HISTORY
Daily routine :
He was a labourer by occupation.
Wakes up at 6 AM
Does household work
Breakfast at 9 AM
Goes to work
Lunch at 2 PM
Returns home 6 PM
Dinner at 8 PM
Sleeps at 9 PM
" Takes Alcohol either in the morning at 10 am or 7 pm in the evening"
PERSONAL HISTORY
Diet: mixed
Appetite: normal
Bowel and bladder movements :Normal
Sleep: adequate
No known allergies
Addictions : chronic alcholic since 30 years
Chronic smoker since 30 years - 1 pack beedi/ day
FAMILY HISTORY
No significant family history
TREATMENT HISTORY
Was on glimiperide for 2 months after getting diagnosed with DM, and stopped using after that, later after 2 months He was on insulin(2.5IU) ,but was not taking insulin regularly
GENERAL EXAMINATION
•Patient is examined in a well lit room after obtaining consent
•Patient is conscious, coherent, cooperative.
Well built and well nourished.
•Mild Pallor
•Icterus,clubbing, cyanosis, koilonychia, edema are absent
•VITALS
Temp- Afebrile
Bp-90/60 mm hg
PR- 82bpm
RR-18CPM
Spo2- 96% on RA
GRBS : 550mg/dl
SYSTEMIC EXAMINATION
RS- bilateral air entry present
CVS : S1, S2 + no murmurs
P/A- soft and non tender
bowel sounds present
CNS : No focal neurological defeicit
HMF intact
Power in B/L upper and lower limb Is 5
Reflexes are present with B/L plantars and flexors
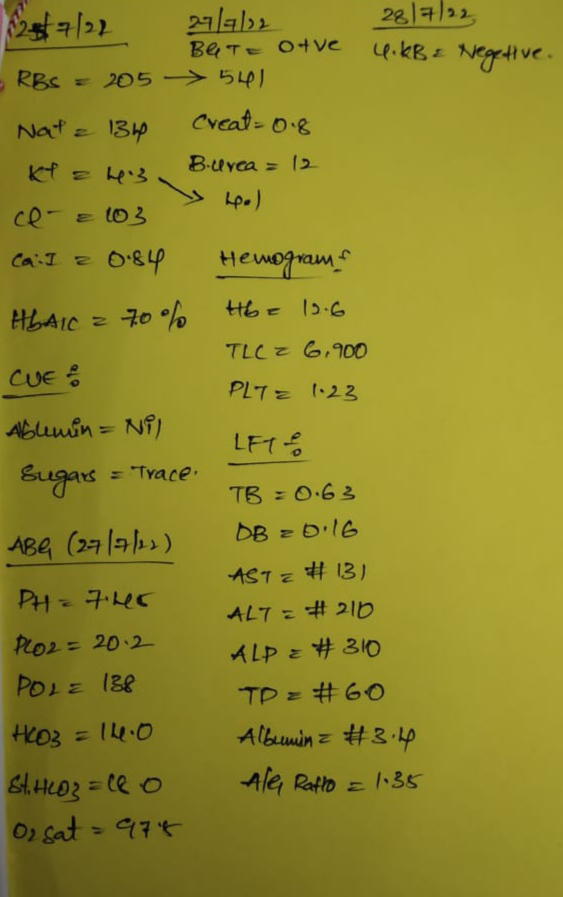
INVESTIGATIONS :
*Fever chart
*PROVISIONAL DIAGNOSIS :
Chronic Alcoholism & Uncontrolled Diabetes DM 2 with Herpes Zoster
*TREATMENT :
√T.THIAMINE PO/OD
√ T. GLIMI - M₁ PO/TIC
√ 70 PROFILE GRBS MONITORING
√ Pre Breakfast , 2hrs After Breakefast
√ Pre Lunch, 2hrs after LunchLunch
√ Pre dinner, 2hrs after dinner
√ 2 AM in the morning
√ INJ HAI 6 Units S/C
√ Pregaba -m 75mg/PO/ HS since 28/7/22
√ Paracetmol 500mg on 3/8/22
√ T.Ultrocet po/od
27/7/22
• Tab.BENFOTIAMINE PO/OD
• TAB.GLIMI -M1 PO/OD
• INJ. HAI 6units S.C
• GRBS monitoring
28/7/22
• Tab.BENFOTIAMINE PO/OD
• TAB.GLIMI -M1 PO/OD
• INJ. HAI 6units S.C
• GRBS monitoring
29/7/22:
.Tab. BENFOTIAMINE PO/BD
Tab. GLIMI -M1 PO/BD
Tab PREGABA- M 75mg
Vitals
29/07/22:
BP 110/70mmHg
PR 68/min
3pm - 325
7pm - 466 - Tab.Glimi 2.5mg
Tab metformin 1g/dl
12am- Hi - HAI units SC
4am - 177
31/07/22:
8am - 239
1am - 348
2pm- 324
4pm-528 Glimi 4mg metformin 1g/dl
10pm-345
2am- Hi Glimi 4mg metformin 1g/dl
01/08/22:
Glimi 4mg metformin 1g/dl
8am-288
10am-352
1pm-200
4pm-394
8pm-338 - Glimi 4mg metformin 1g/dl
11pm-333
2am-336
02/8/22 :
Glimi 4mg metformin 1g/dl
8am-155
11:30am -318
5:00pm-394
8:00pm- 338
10:30pm-477
2:00am-362
03/08/22:
8:00am-135
12pm - 300
8pm - 532
10pm - 411
2am - 320
04/08/22:
8am - 176
06/08/22:
10:30 am-272
























Comments
Post a Comment