his is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
M varshith
Roll no 85
8 th semester
Bowel and bladder movements- regular
No known allergies
Addictions- used to consume pan one or twice daily but stopped from past 4 months.
Daily routine-she'll wake up around 5:00am and completes her household chores and then have breakfast at 10am and goes for work then will have ,lunch at 2:00pm and comes back from work around 5pm and will have tea .Then she'll have her dinner at 8pm .Mostly all the three times she'll have rice .Then she'll go to bed by 10pm
FAMILY HISTORY- not significant
GENERAL EXAMINATION-patient is conscious, coherent, cooperative. Well oriented to time , place and person, moderately built and moderately nourished
Vitals -
BP- 130/80 mmHg
PR- 92 bpm
RR- 18 cpm
TEMP- 98.2 F
PRESENCE OF PALLOR.-NO SIGNS ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, OEDEMA.
SYSTEMIC EXAMINATION-
1) CVS- S1, S2 heard, no murmurs.
2) RS- BAE present, NVBS
3) PER ABDOMEN- diffuse tenderness
no organomegaly
4) CNS:
Higher mental functions - intact
Cranial nerves - intact
Motor examination - normal
Sensory examination:Normal
No meningeal signs
INVESTIGATIONS-
Ecg
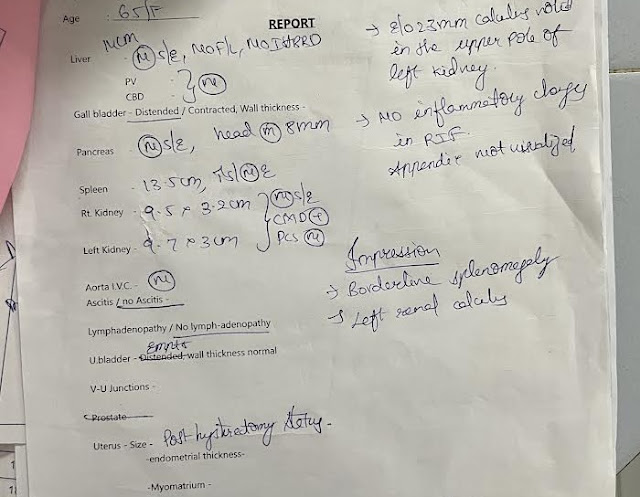
ULTRASOUND-
Chest x ray

PROVISIONAL DIAGNOSIS-
PYREXIA UNDER EVALUATION WITH LEFT LOWER ZONE COLLAPSE.PRE RENAL ACUTE KIDNEY INJURY.HYPOKALEMIA SECONDARY TO GE.
TREATMENT-
1. INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV /TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. NEOMOL 1GM IV/SOS
5. TAB. DOLO 650MG PO/TID
6. SYP. ASCORIL-LS 15ML/PO/TID.
1/10/2023
2. INJ. ZOFER 4MG IV/TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. NEOMOL 1GM IV/SOS
5.INJ.MONOCEF -1GM IV/BD
6. TAB. DOLO 650MG PO/TID
7. SYP. ASCORIL-LS 15ML/PO/TID.
2/10/2023
1.INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. NEOMOL 1GM IV/SOS
5.INJ.KCL 2AMPULES IN 500ML NS IV SLOWLY OVER 5-6HOURS
6.TAB.PCM 650MG PO/TID
7.TAB.AMLODIPINE 5MG PO/OD
8.SYP.ASCORIL-LS 15ML/PO/TID.
9.INJ.CIPROFLOXACIN 200MG IV/BD
10.TAB.SPORLAC DS PO/TID
3/10/2023
1.INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. PCM 1GM IV/SOS
5.INJ.REDOTRIL 100MG PO/BD
6.TAB.PCM 650MG PO/TID
7.TAB.AMLODIPINE 5MG PO/OD
8.SYP.ASCORIL-LS 15ML/PO/TID.
9.INJ.CIPROFLOXACIN 200MG IV/BD
10.TAB.SPORLAC DS PO/TID
11.INJ.METROGYL 500MG IV/TID
4/10/2023
1.INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. PCM 1GM IV/SOS
5.INJ.REDOTRIL 100MG PO/BD
6.TAB.PCM 650MG PO/TID
7.TAB.AMLODIPINE 5MG PO/OD
8.SYP.ASCORIL-LS 15ML/PO/TID.
9.INJ.CIPROFLOXACIN 200MG IV/BD
10.TAB.SPORLAC DS PO/TID
11.INJ.METROGYL 500MG IV/TID
5/10/2023
1.INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. PCM 1GM IV/SOS
5.INJ.REDOTRIL 100MG PO/BD
6.TAB.PCM 650MG PO/TID
7.TAB.AMLODIPINE 5MG PO/OD
8.SYP.ASCORIL-LS 15ML/PO/TID.
9.INJ.CIPROFLOXACIN 200MG IV/BD
10.TAB.SPORLAC DS PO/TID
11.INJ.METROGYL 500MG IV/TID
6/10/2023
1.INJ. PAN 40MG IV/OD
2. INJ. ZOFER 4MG IV/TID
3. IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
4. INJ. PCM 1GM IV/SOS
5.TAB.AMLODIPINE 5MG PO/OD
6.TAB.PCM 650MG PO/QPD
7.SYP.ASCORIL-LS 15ML/PO/TID.
8.INJ.DOXYCYCLINE 100MG IV/BD
9.TAB.SPORLAC DS PO/TID
10.INJ.SODIUM BICARBONATE 25MCG IV
7/10/2023
1.IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
2.INJ.DOXYCYCLINE 100MG IV/BD
3.INJ.FALCIGO 120MG IV
4.INJ.SODIUM BICARBONATE 50MCG IV STAT 50 MCG IN 500ML NS OVER 8HOURS
5.INJ.PCM 1G IV/SOS
6.INJ.ZOFER 4MG IV/SOS
7.TAB. PCM 650MG PO/QID
8.TAB.NODOSIS 500MG PO/QID
9.TAB.AMLODIPINE 5MG PO/OD
10.INJ.PAN40MG IV/OD
8/10/2023
1.IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
2.INJ.DOXYCYCLINE 100MG IV/BD
3.INJ.FALCIGO 120MG IV
4..INJ.PCM 1G IV/SOS
5.INJ.ZOFER 4MG IV/SOS
6.TAB. PCM 650MG PO/QID
7.INJ.PAN40MG IV/OD
8.TAB.NODOSIS 500MG PO/QID
9.TAB.AMLODIPINE 5MG PO/OD
9/10/2023
1.IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
2.INJ.DOXYCYCLINE 100MG IV/BD
3.INJ.METHYLPREDISOLONE 1GM IV/OD
4.INJ.PAN40MG IV/OD
5.TAB.NODOSIS 500MG PO/QID
6.INJ.LASIX 20MG IV/BD
7.INJ.KCL 2AMPULES IN 500ML NS IV SLOWLY OVER 5-6HOURS
11/10/2023
1.IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
2.INJ.DOXYCYCLINE 100MG IV/BD
3.INJ.METHYLPREDISOLONE 1GM IV/OD
4.INJ.PAN40MG IV/OD
5.TAB.NODOSIS 500MG PO/QID
6.INJ.LASIX 20MG IV/BD
7.SYP.ASCORIL-LS 10ML/PO/TID.
12/10/2023
1.IV. FLUIDS - 2NS @ 75ML/HR - 1 RL
2.INJ.DOXYCYCLINE 100MG IV/BD
3.INJ.METHYLPREDISOLONE 1GM IV/OD
4.INJ.PAN40MG IV/OD
5.TAB.NODOSIS 500MG PO/QID
6.INJ.LASIX 20MG IV/BD
7.SYP.ASCORIL-LS 10ML/PO/TID.

Comments
Post a Comment